Incisional Hernia: Causes, Symptoms And Treatments
Incisional hernia (IH) is a common complication after abdominal surgery. After laparotomy – opening the abdomen in an operating room – the chances of developing this type of hernia in the first year are 5 to 15%. This percentage is biased, since 35% of them are diagnosed up to 5 years after the operation.
On the other hand, the repair of an incisional hernia is not always satisfactory, since up to 44% reappear. If you want to know everything about this complex clinical entity, read on.
What is an incisional hernia?
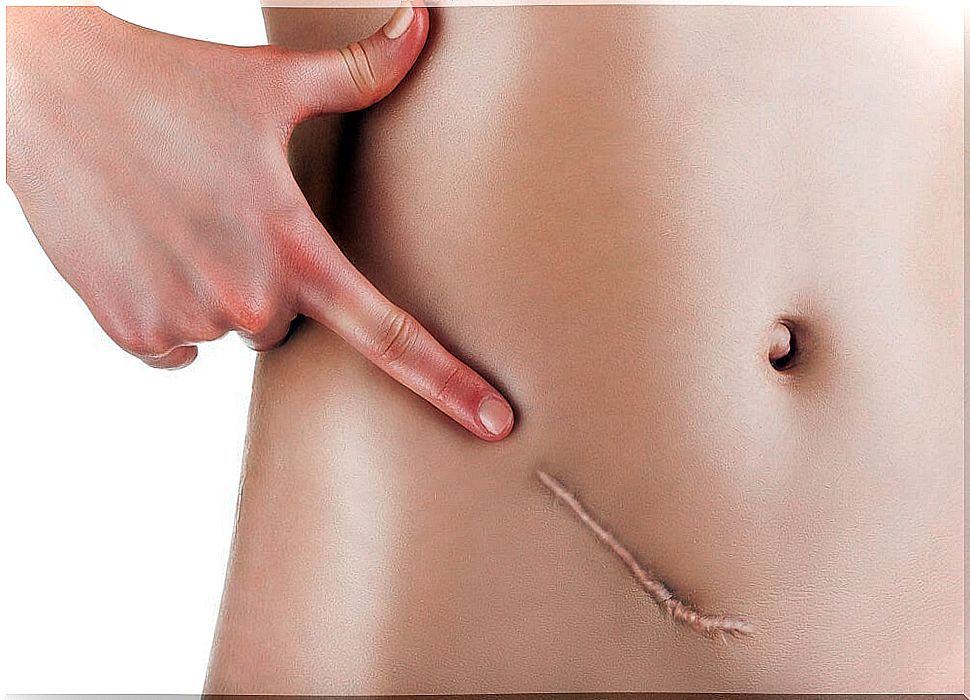
A hernia is defined as the protrusion of any organ outside the cavity in which it is normally housed. In this case, the incisional form is an abnormal protrusion of the peritoneum – membrane that covers the inner wall of the abdomen – through the pathological scar of a surgical or traumatic wound.
As we have said, up to 15% of patients who have undergone abdominal surgery will develop IH. 50% of these problems are diagnosed during the first year after the operation, while another 35% can be detected up to 5 years later, according to studies.
In some surgical clinics, up to 8% of patients on the waiting list present with symptoms of an incisional hernia. These data show that it is a much more common and annoying medical problem than it first seems.

Types of incisional hernias
There are many types of HI, depending on the qualifying criteria you want to follow. The Cuban Journal of Surgery shows us the most important:
- Depending on its etiology or underlying cause: an incisional hernia can be postlaparotomy, posttraumatic, trocar, tacker, and other synonyms.
- Based on its evolution time: it can be a recent or old HI. As we have said, up to a third of them are diagnosed 5 years later.
- According to its location: there are many types of IH based on its place of appearance. They can be in the groin, upper stomach, belly button, at the site of a surgical scar, and several other places.
- Based on the diameter and the hernial ring: an HI is small if its diameter is less than 5 centimeters. It is considered monstrous (according to the clinical term) if the diameter exceeds 20 centimeters.
There are many more classification criteria to classify an incisional hernia, but with these examples its physiological complexity is more than clear. In addition, depending on the location and size, they may or may not alter the rhythm of the gastrointestinal tract, leading to very diverse symptoms.
What are the symptoms?
The Drugs portal shows us some of the typical symptoms of an incisional hernia. Among them we find the following:
- Abdominal pain, which varies depending on where the hernia occurs.
- Nausea and vomiting.
- Swelling or soft lump, especially located at the site of a previous abdominal incision.
- Generalized abdominal bloating.
Without a doubt, the clearest symptom of an IH is a kind of lump or protrusion in the place where a surgical intervention has been performed before. Although it can appear anywhere, it is more likely to occur in incisions that are located in the area of the sternum to the pubis.
Possible complications
Older age, being obese, generalized malnutrition, a previous infection in the incision area, smoking, and certain medications can worsen the clinical picture of an incisional hernia.
As unpleasant as it may sound, there are isolated cases in which an IH is so large and obvious that it can cause an epidermal tear and bowel leakage from the incision site.
What Causes an Incisional Hernia?
As we have said, in most cases incisional hernias appear from previous laparotomies. These types of wounds behave worse than others on a clinical level. In the first place, as studies indicate, they are lesions that do not remain at rest after surgery, since respiratory movements do not allow total healing.
Abdominal movements and other problems make healing from a laparotomy difficult, so the sutured line will never come to the preoperative strength that characterized it. After 1-2 months of the intervention, it is estimated that the tissue can reach 50% of its viability.
The presence of this weak tissue promotes the protrusion of the peritoneum, or what is the same, the appearance of an incisional hernia.
How is it diagnosed?
In many cases, the incisional hernia is reducible. This means that the patient can notice it only when performing activities that cause a clear abdominal pressure, such as coughing, sneezing, exercising or lifting a heavy object.
However, if the incisional hernia is visible to the eye of the medical professional, no further tests are usually necessary, other than routine palpation. In cases that raise doubts, you can go to computed tomography scans.
Treatment of an incisional hernia
There are several fronts to approach an HI. Among all the possible ones we find the following:
- Medications: Non-steroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, help reduce pain, inflammation, and possible secondary low-grade fever. Anyway, you should ask your doctor if these drugs are for you.
- Hernia reduction: Hernias are pushed directly without the need for surgery. Certain medications that cause muscle strain, making pushing easier, may be necessary.
- Surgery: due to its complexity, we dedicate our own lines to it in the following section.
Incisional hernia surgery
As the Memorial Sloan Kettering Cancer Center indicates , in many cases the only solution to repair HI is to undergo surgery. Depending on the diameter of the hernia and the patient’s condition, a laparoscopy or open surgery may be performed.
In laparoscopic surgery, the surgeon will make a series of strategic cuts in the abdomen and will swell the cavities of the patient to observe the organs well. Using a thin scope with light and instruments, the professional will close the hernia and return all the structures to their place.
In open surgery, as the name suggests, a large incision is made in the abdomen to repair the hernia. The surgeon may choose to place an abdominal patch as a support (mesh) to prevent a re-protrusion. Over time, this patch is reabsorbed into the patient’s tissue.
The results of these interventions are not always satisfactory. Recurrence rates for incisional hernias after repair range from 31% to 44%.
Tips and Recommendations
As you can imagine, only a professional can fix an incisional hernia, but this does not mean that certain precautions cannot be taken from home to prevent it from getting worse.
In conclusion, we present some of the things you can do on a day-to-day basis if you have an HI:
- Maintain a healthy weight: being overweight increases the pressure in the abdominal cavities and, therefore, favors the ejection of the hernia to the outside. It is necessary to consult with the doctor if the patient should undergo diets once he has received the diagnosis.
- Do not strain in the bathroom: intestinal efforts can cause the symptoms of the hernia to worsen. Drinking lots of water and a high fiber diet can help you a lot.
- Do not smoke: smoking promotes the appearance of coughs and sputum, among many other negative things. The more you cough, the more your chest will hurt and the hernia will eject.
- Return to your normal activities when the doctor indicates it: it is necessary to maintain prolonged rest.
Incisional hernias are complications of other disorders
An incisional hernia is a common clinical event in people who have had abdominal surgery. Although it is not an extremely worrisome clinical entity, getting rid of it can be a complicated task, since the affected tissue does not usually respond well to repair processes.
If you have an incisional hernia, it is best to put yourself in the hands of professionals and be patient. Various medications and lifestyle changes can greatly improve your symptoms, so don’t despair.