Transcutaneous Cardiac Pacemaker: In Which Patients Are They Indicated?
The transcutaneous cardiac pacemaker is a device used to treat arrhythmias. It is an interim measure in the treatment of bradyarrhythmias (arrhythmias where the heart rate is slower than normal) and some tachyarrhythmias (arrhythmias where the heart rate is faster than normal).
The ultimate goal of this pacemaker is to ensure that blood reaches the entire body correctly. This concept in physiology is called cardiac output and is the product of heart rate and stroke volume.
In other words, it is calculated by multiplying the number of beats in a minute by the mL of blood that the heart ejects into the body in each beat.
Transcutaneous versus transvenous cardiac pacemaker
In general, when we talk about transcutaneous pacemakers we refer to temporary devices. These are transitory paces that are located externally in an emergency situation.
The most common is that they are implanted in out-of-hospital emergencies until the study is carried out to establish the definitive treatment. In addition, they can also be used during invasive processes in patients with risk factors, such as coagulopathies.
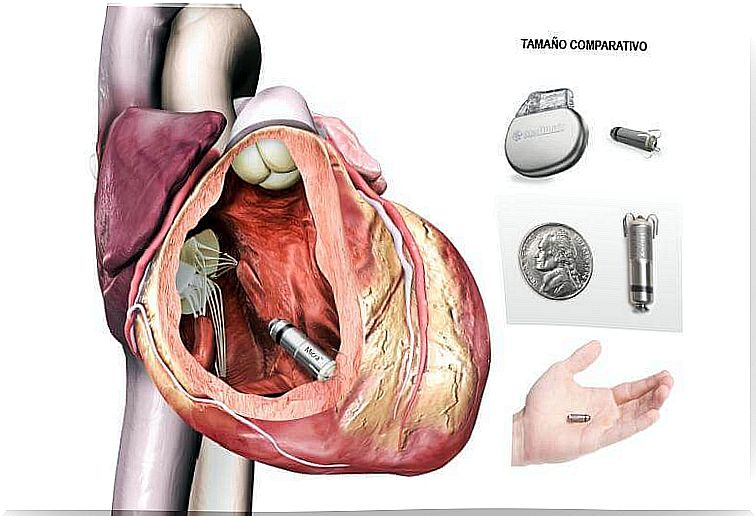
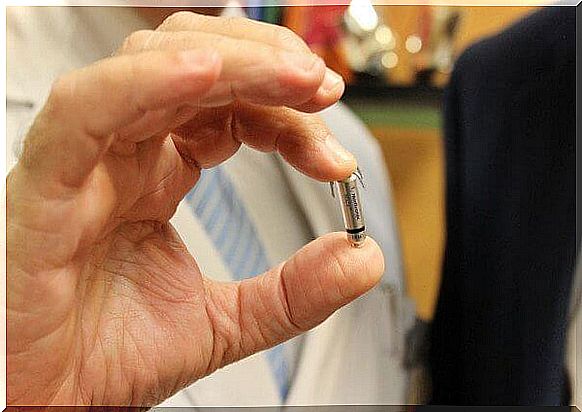
There is another type of pacemaker, the so-called “transvenous” or “endocavitary” and which are definitive devices, which are placed inside the chambers of the heart, generally in the right ventricle.
Where is the transcutaneous cardiac pacemaker implanted?
The transcutaneous cardiac pacemaker is located in regions of venous access within the heart chambers.
According to the anatomy of the heart, we could consider that this organ is divided into 4 chambers (2 upper and 2 lower). In turn, these constitute 2 halves of the heart (left heart and right heart).
Broadly speaking, the right heart is defined as the portion responsible for transporting venous blood, poor in oxygen and rich in carbon dioxide. For its part, the left heart receives renewed blood from the lungs and sends it to the rest of the body through the aorta.
The transcutaneous pacemaker is implanted in the right heart. The electrical catheter is inserted through a central venous access. It can be through the superior vena cava from the shoulder or through the inferior vena cava through the femoral vein. The most common is to create a route from the right internal jugular vein and, in case of failure, the left subclavian vein would be chosen.
The ideal area to place the pacemaker is the apex of the right ventricle. That is, place it at the tip of the ventricle next to the trabeculae. It has to be this region and not another.
The reason is that the most frequent complication in the implantation process of the pacemaker is that it moves and adopts an abnormal position that can perforate the walls of the tissue where it is lodged.
It is essential to avoid damaging the tricuspid valve, since this membrane separates the blood from the atrium (upper chamber) from the ventricle (lower chamber). This is important so that the beat occurs correctly and there is enough time for the filling and subsequent contraction of each chamber without backflow of blood.
When is it indicated?
The clearest indication for the use of a transcutaneous cardiac pacemaker is to have an arrhythmia. In this group of electrical disorders, the heart contracts abnormally. It may be because the rhythm is inappropriate or it occurs in a disorderly way. Therefore, the blood cannot reach the rest of the body.
It is essential to perform an electrocardiogram (ECG) on the patient in situations of rest and stress to assess changes in the recording of waves.
In addition, the study is usually accompanied by imaging tests that analyze the quality of the right ventricle. The most common indications for a transcutaneous cardiac pacemaker are the following:
- Asystolia
- Torsade des Puntes.
- Complete AV block.
- Recurring sinus pauses.
- Failure of another previous pacemaker.
- Ventricular arrhythmias induced by drugs.
- Acute myocardial infarction with bilateral bundle branch block.
- Alternating left bundle branch and right bundle branch block.
- Right bundle branch block with anterior / posterior alternation.
- Acute right ventricular myocardial infarction with bradyarrhythmia.
- Atrial or ventricular overstimulation during ventricular tachycardias.
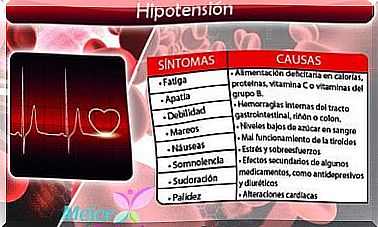
- Symptomatic bradycardia (can be sinus with hypotension or AV block that does not respond to atropine).
If the doctor has told you that you should have a pacemaker, take into account all his indications both before and after the procedure so that everything goes correctly and you can feel well. Of course, do not forget to always maintain good lifestyle habits to provide more benefits to your body.